Treatment of Adolescent Scoliosis
Each case of scoliosis, defined as three-dimensional curvature of the spine, is as unique as the person who has the condition. If the size of the curve is less than 25 degrees in the growing child, periodic observation by us is sufficient. Wearing an orthotic brace is beneficial if the curve reaches 25 degrees or more in a growing child with immature bones. Bracing can come in the form of a traditional TLSO (Boston brace) or dynamic SpineCor brace. The role of physiotherapy or chiropractic manipulation is still controversial. When the curve measures more than 40 to 45 degrees in the growing child, and more than 50 degrees in the skeletally mature patients, surgery may be the best treatment.
Surgical Approaches
Scoliosis surgery aims to arrest the progression of the curve, while at the same time making a curved spine straighter. It
is important to try to preserve as much of the spine’s natural mobility as possible.
For many patients, scoliosis surgery is done from the back or posterior approach i.e. posterior spinal fusion with instrumentation. Bone is taken from another part of the patient’s body (either local sources, ribs, or the pelvis) and then grafted onto the vertebrae. The bone graft will take at least one year to “harden” to the vertebrae. Nowadays, we routinely take the bone from the ribs so that we can at the same time reduce the rib hump deformity. To stabilize the fusion and hold the vertebrae in place during this time period, two titanium rods are attached to the spine with hooks or pedicle screws or both. For stiff and large curves, we may elect to use cobalt-chromium rods instead, which are stronger than titanium rods.
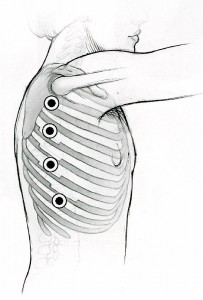
Sometimes the best approach is from the front, or anterior region. This maybe possible if the patient only presents with one significant curve. In this type of surgery, the incision is made through the chest and/or abdominal cavity. If the curve is in the chest, we may perform thoracoscopic surgery – a type of minimally invasive surgery-to correct scoliosis. This technique is possible because of good images provided by the camera connected to the thoracoscope. This technique results in smaller incisions (four one-half inch incisions on the side of the chest wall compared with one 10-inch incision with traditional front approach, and also avoiding a long scar at the centre of the back compared with the traditional
posterior spinal fusion and instrumentation). It is particularly suitable for patients who have scoliosis confined to the thoracic spine or where the spine can be reached through the chest cavity. Other requirements include curves which are right sided. In this procedure, the
patient is placed on her or his side. The right lung is temporarily deflated by the anesthetist for the duration of the surgery. The procedure involves removing the discs between the vertebrae so that the spine becomes “looser”. The spaces are then filled with bone taken from the ribs. Titanium screws will then be inserted under radiographic control. A rod will be used to connect the screws, and by doing so straightens the spinal curve. The picture below illustrates the small incisions used in this form of minimally invasive spine surgery.
There are times when a combined anterior and posterior (from behind) approach is used, if the curve is too big and rigid. Generally, we will first approach the front to “loosen” the spine by removing the discs between the vertebrae. The second stage will
involve opening the back of the spine, and correcting the scoliosis using a combination of hooks or screws, although the tendency is to use all screws nowadays as they offer better stability than hooks.
Generally speaking, scoliosis surgery requires 4 to 5 hours in the operating room and a hospital stay of about 5 to 7 days. Most patients return to school or work 2 to 4 weeks after surgery; sporting activities can be resumed at about 12 months post-surgery.
The pictures below show the x-rays of a patient who had severe scoliosis before and after surgery.
Neurophysiological Monitoring
One of the risks of scoliosis surgery is injury or damage to nerves contained within the spinal cord. Specifically, though unlikely, there is a chance of paralysis. Traditionally, the patient is awakened during surgery to ensure that the nerves are unharmed and movement is normal. We routinely use neurophysiological or intraoperative nerve monitoring, where wire leads are connected from the patient’s foot or leg to the skull. A technician constantly monitors
the nerve activity, which is detectable through these leads throughout the operation. We also perform the traditional “wake-up” test if required.
Blood product support
Scoliosis surgery potentially involves significant blood loss. During surgery, blood can be conserved by using meticulous technique and state-of-the-art surgical instruments to stop or prevent excessive bleeding. In many cases, blood lost during a surgical procedure can be salvaged and recycled using cell savers. Certain medications maybe administered by our anesthesiologist to reduce intraoperative bleeding e.g. tranexamic
acid. Occasionally, we will get the patients to donate their blood before the surgery to be re-transfused back to themselves during or after the surgery (autologous transfusion).
Summary
For surgeries as complex as those used to correct scoliosis, there’s no substitute for an experienced health care team, from the surgeons who specialize in spinal surgery,nurses in the wards, physiotherapists who provide chest physiotherapy and ambulatory physiotherapy. We
offer scoliosis patients:
- Comprehensive counseling before and after surgery.
- A comprehensive approach to the non-operative and operative treatment
- Availability of highly qualified spine surgeon to perform the surgery
- The use of high-quality fluoroscopic (X ray) images during surgery
- Intraoperative nerve monitoring
- Excellent post-operative care at our paediatric high-dependency and intensive care unit if required
X rays of a patient who had thoracoscopic fusion and instrumentation of thoracic scoliosis
Contributing Specialist:
Dr Hee Hwan Tak
MBBS, FRCS (Ed), FRCS (Glas), FAMS (Ortho)
Medical Director and Senior Consultant, Pinnacle Spine & Scoliosis Centre
Mobile: 65-98283132
Tel: 65-67370680
Fax: 65-67370522
Emergency: 65-97718964
Website: http://www.p-ortho.com
3 Mount Elizabeth, Mount Elizabeth Medical Centre, #04-07, Singapore 228510
Adjunct Associate Professor, Nanyang Technological University, Singapore
Panel of Medical Experts, The Subordinate Courts of Singapore
Associate Editorial Board Member, The Spine Journal (USA)